Hair Transplant For People With Scalp Skin Conditions
Hair transplantation can be possible for some people with scalp skin conditions, but timing matters. Active inflammation, open lesions, or untreated infections can reduce graft survival and raise the risk of flare-ups. A dermatologist-led plan that brings the condition under control first is the safest way to decide if and when surgery makes sense.
When Hair Loss Is Linked To A Skin Disease
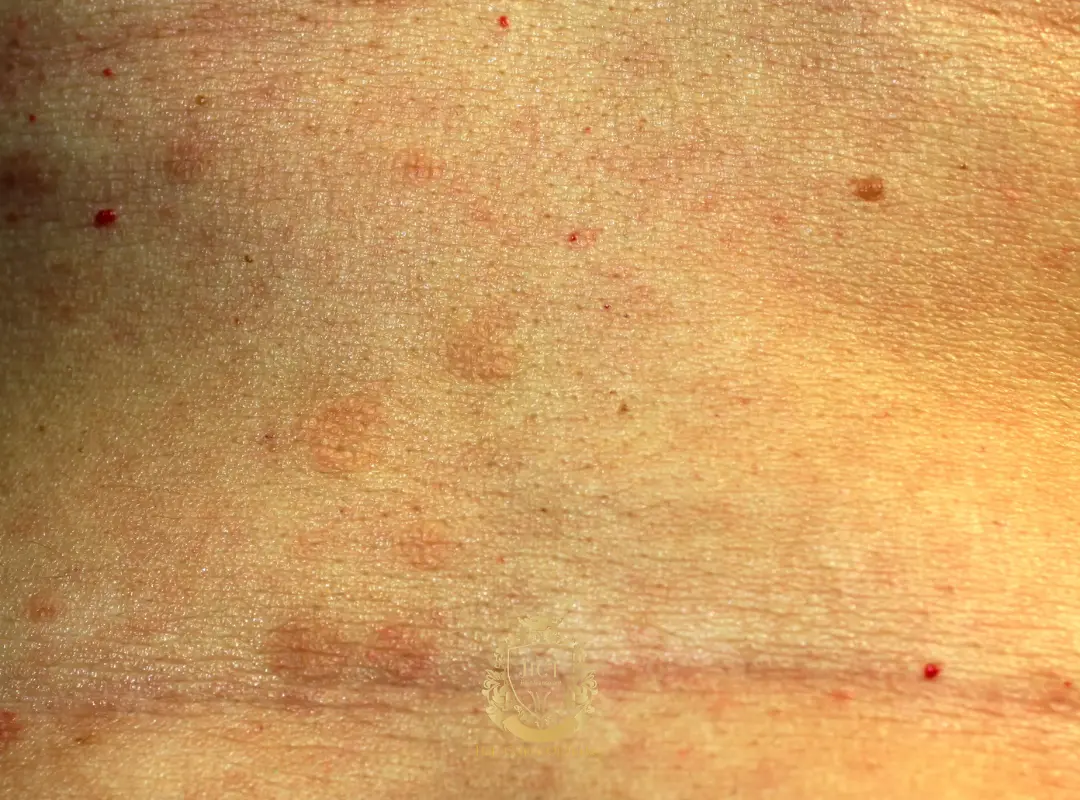
Many scalp conditions can irritate the skin, disrupt the hair cycle, or damage follicles over time. Some cause temporary shedding from inflammation or scratching, while others can lead to permanent loss if scarring develops. Before planning a hair transplant, the first step is confirming what type of hair loss you have and whether the scalp is stable.

Can You Get A Hair Transplant If You Have A Scalp Condition?
In many cases, yes—but only when the condition is well controlled and the scalp is calm. Transplanting into skin that is inflamed, infected, or actively forming plaques or erosions can compromise healing and graft survival. For scarring (cicatricial) alopecia, surgery may be contraindicated unless the disease has been inactive for a prolonged period and your dermatologist agrees.
Key Safety Checks Before Surgery
Dermatology Clearance
A dermatologist should confirm the diagnosis and control the condition with an appropriate treatment plan. If the diagnosis is uncertain, dermoscopy and sometimes a scalp biopsy can be needed, especially when scarring alopecia is suspected.
No Active Infection Or Open Lesions
Bacterial infections, pustules, oozing areas, or untreated fungal infections must be treated first. Surgery is usually delayed until the scalp surface has healed and any contagious condition has cleared.
Stability In The Recipient And Donor Areas
Both the area to be transplanted and the donor zone (usually the back and sides of the scalp) should be free of active disease. If either area is affected, graft harvesting or placement can be more difficult and may trigger worsening symptoms.

Psoriasis
Scalp psoriasis is an immune-mediated condition that can flare with irritation or trauma. Many patients can still be candidates when plaques and itching are under control and there are no open cracks or bleeding lesions. Planning surgery during a stable phase and coordinating aftercare with your dermatologist reduces avoidable risk.

Seborrheic Dermatitis
Seborrheic dermatitis often causes greasy scaling and itching on the scalp. It does not usually cause permanent hair loss, but scratching and inflammation can increase shedding. Hair transplantation is typically scheduled after symptoms are brought under control with a consistent scalp-care routine.

Tinea Capitis (Scalp Ringworm)
Tinea capitis is a contagious fungal infection that is more common in children. It can cause scaly patches, broken hairs, and sometimes painful swollen areas (kerion) that may scar. Hair transplantation is not performed during infection; treatment must be completed and the scalp should be re-evaluated after clearance.
Lichen Planopilaris And Other Scarring Alopecias
Lichen planopilaris is an inflammatory scarring alopecia that permanently destroys follicles when active. Active disease is generally considered a contraindication for hair transplantation. In selected cases, transplant may be discussed only after a long period of inactivity and with clear expectations, since relapse remains possible.

Vitiligo
Vitiligo causes loss of pigment cells, leading to lighter patches on skin and sometimes hair. Because skin trauma can trigger new patches in some people (the Koebner phenomenon), any surgical procedure requires careful risk–benefit discussion. If vitiligo is stable and your dermatologist agrees, a transplant may be considered, but it is approached cautiously.

Alopecia Areata
Alopecia areata is an autoimmune condition that can cause sudden, patchy hair loss. Surgery is often avoided because the condition can relapse unpredictably and may affect overall satisfaction with results. In rare, carefully selected cases with long-term stability, a dermatologist may consider transplantation, but medical options are usually explored first.
Preparing For A Consultation
Bring a list of your scalp symptoms, previous diagnoses, and any creams, shampoos, or tablets you use. Share flare triggers such as stress, infections, or new products, and mention any autoimmune or endocrine conditions. Expect your clinician to explain whether your hair loss is reversible shedding or permanent loss, and what results are realistic for your scalp health.
Our Approach At Hair Center of Turkey
At Hair Center of Turkey, candidates with scalp conditions are assessed together with a dermatologist, an anaesthesia doctor, and an experienced hair transplant team. If a condition is active, the priority is stabilising the scalp first and planning surgery only when it is medically appropriate. If you want a personalised assessment, you can contact our clinic for a consultation and medical review.
FAQ
Can I Have A Hair Transplant If I Have Psoriasis?
Often, yes—if your psoriasis is controlled and there are no active plaques, cracks, or open lesions in the donor and recipient areas. Your dermatologist should confirm stability and advise on pre- and post-op scalp care.
Is Hair Transplantation Possible With Seborrheic Dermatitis?
It can be, but it’s usually planned after symptoms are controlled. A calm scalp reduces itching, flaking, and irritation during healing.
Can I Get A Transplant If I Had Scalp Ringworm (Tinea Capitis)?
Not during an active infection. Complete antifungal treatment first and have your scalp rechecked. If scarring occurred, your clinician will discuss whether transplantation is realistic.
Is Hair Transplant Suitable For Lichen Planopilaris?
Active lichen planopilaris is generally a reason to postpone surgery. A transplant may be considered only after long-term inactivity under dermatologist supervision, with careful expectations about recurrence risk.
Is A Hair Transplant Safe For Vitiligo?
It depends on stability and your tendency to develop new patches after trauma. A dermatologist can help assess your risk and whether a cautious approach is reasonable.
Does A Hair Transplant Work For Alopecia Areata?
It’s usually not the first choice because the condition can flare and affect results. If the disease has been stable for a long time, a specialist may discuss it case by case.