Types Of Hair Loss In Women
Most women shed some hair every day—often around 50 to 100 strands. Hair loss becomes more likely when shedding noticeably increases for weeks, the part line widens, or patchy bald spots appear. Because the causes range from stress to hormones and autoimmune disease, a dermatologist can confirm the type and recommend the safest treatment.
What Counts As Hair Loss Vs Normal Shedding
It’s normal to shed hair daily as part of the growth cycle. Many people lose roughly 50 to 100 hairs a day, and long hair can make shedding look more dramatic than it is.
Consider medical advice if shedding is consistently much higher than your usual baseline, if you’re losing clumps when washing or brushing, or if you notice thinning that isn’t improving after a few months.
What Is Hair Loss In Women
Hair loss in women (alopecia) happens when more hair falls out than grows back. It may show up as diffuse thinning, a widening part, a receding hairline around the temples, or distinct bald patches.
Hair can be fine, light vellus hair or thicker terminal hair. Changes in the balance between these hair types can also affect overall density and how full the hair looks.
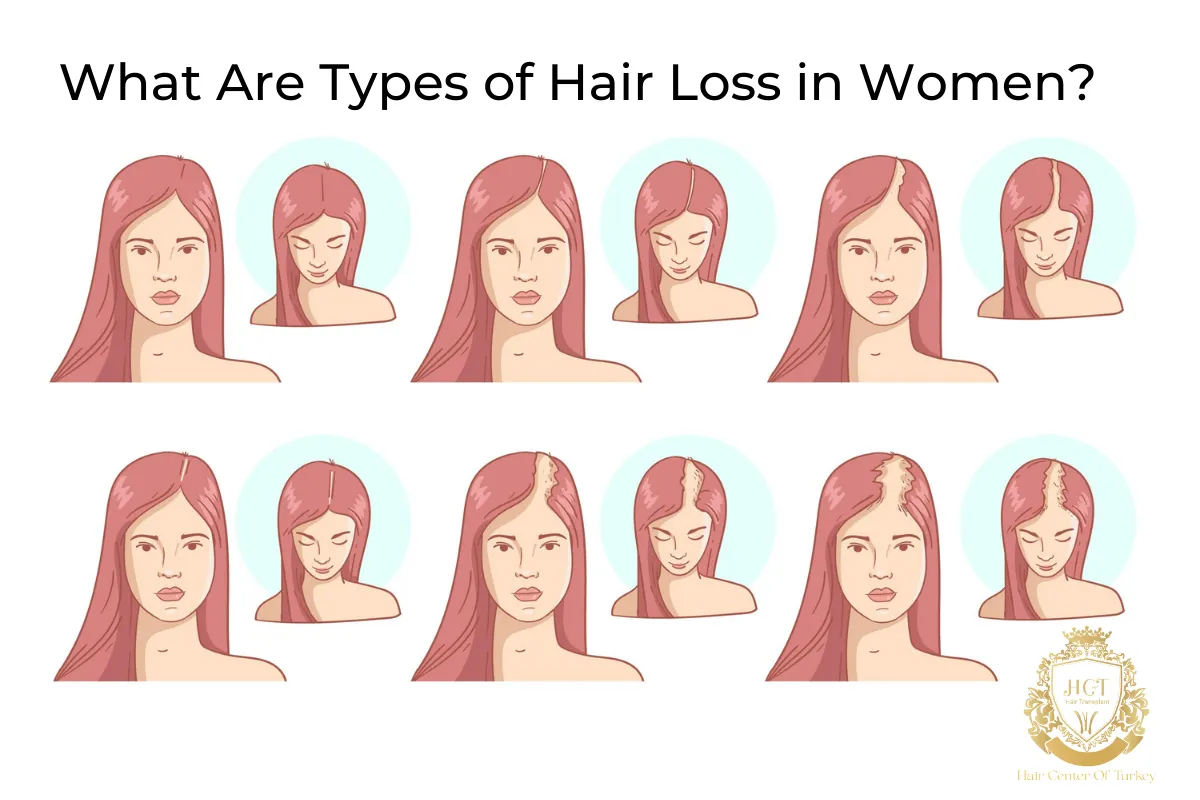
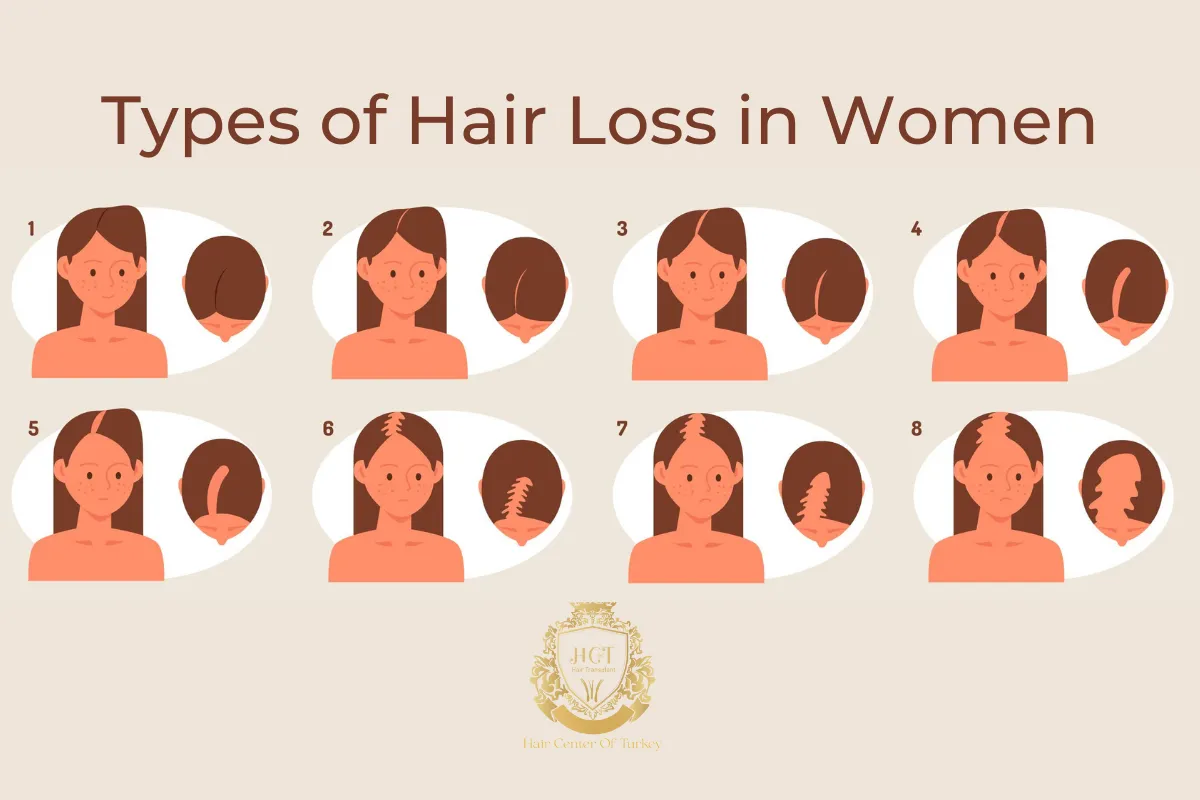
Common Types Of Hair Loss In Women
Female Pattern Hair Loss (Androgenetic Alopecia)
Female pattern hair loss is the most common cause of long-term thinning in women. It often looks like a gradually widening part or reduced density on the crown while the frontal hairline stays mostly intact.
Genetics and hormone sensitivity play a role. The condition can progress slowly, so early evaluation helps you choose options that fit your goals and medical history.
Telogen Effluvium
Telogen effluvium is a common reason for sudden, diffuse shedding. A trigger pushes more hairs than usual into the resting (telogen) phase, and shedding becomes noticeable weeks to months later.
Typical triggers include significant stress, illness, surgery, rapid weight loss, childbirth, and medication changes. Many cases improve once the trigger is addressed, but persistent shedding should be assessed.
Anagen Effluvium
Anagen effluvium is rapid hair loss during the growth (anagen) phase. It is most often linked to chemotherapy and some other medical treatments that affect fast‑growing cells.
Hair usually starts to regrow after treatment ends, though texture or density can change during recovery.
Alopecia Areata
Alopecia areata is an autoimmune condition that causes sudden, round or oval bald patches. Some people feel itching or tenderness before hair sheds.
It can be unpredictable: hair may regrow and then fall out again. A dermatologist can confirm the diagnosis and discuss treatment options, including anti‑inflammatory therapies.
Traction Alopecia
Traction alopecia comes from repeated tension on the hair, often from tight ponytails, braids, extensions, or certain headwear.
Catching it early matters. Changing hairstyles and reducing tension can help prevent permanent thinning, especially around the hairline and temples.
Traumatic Hair Loss (Including Trichotillomania)
Some hair loss is caused by physical damage, friction, or compulsive pulling (trichotillomania). Breakage may look like thinning, but the underlying issue is mechanical rather than hormonal.
Supportive care can include gentler styling, scalp protection, and, when needed, mental‑health support for hair‑pulling behaviors.

Scarring (Cicatricial) Alopecia
Scarring alopecias damage hair follicles and can lead to permanent hair loss. Symptoms may include scalp pain, burning, redness, scaling, or a smooth shiny area where follicles are no longer visible.
These conditions require prompt dermatology care because early treatment can slow or stop further follicle damage.
Alopecia Universalis
Alopecia universalis is a severe form of alopecia areata with loss of most or all scalp hair and often body hair.
It’s less common, but it benefits from specialist care because treatment and follow‑up are different from more localized patchy hair loss.
Symptoms Of Hair Loss In Women
Hair loss doesn’t look the same for everyone. Some women notice gradual thinning over years, while others see sudden shedding over weeks.
Common signs include a widening part, reduced ponytail thickness, more visible scalp on the crown, or distinct bald patches. Scalp itching, tenderness, scaling, or pain can signal inflammation and should be checked.
Common Causes And Risk Factors
Hair loss can be triggered by a mix of genetic, hormonal, medical, and lifestyle factors. Hormonal shifts (postpartum changes, perimenopause, menopause), thyroid disorders, iron deficiency anemia, chronic illness, and autoimmune disease are frequent contributors.
Medications and supplements can also play a role. Rapid dietary changes, significant weight loss, and ongoing stress may affect the hair cycle, especially in telogen effluvium.
Harsh chemical processing and frequent heat styling can weaken hair shafts and worsen breakage, which may make thinning look more severe.

How Dermatologists Diagnose Hair Loss
A dermatologist typically reviews your medical history, recent stressors and illnesses, hair‑care habits, and family history. They examine the scalp and hair distribution, looking for inflammation, scarring, broken hairs, and pattern changes.
Depending on the presentation, testing may include a hair‑pull test, dermoscopy (a magnified scalp exam), blood tests (such as thyroid and iron studies), and sometimes a scalp biopsy.
Treatment Options
The right treatment depends on the cause. Some situations improve with time and trigger management, while others respond best to medical therapy or procedures.
Common strategies include reducing traction and harsh styling, correcting nutritional deficiencies under medical guidance, and treating underlying conditions such as thyroid disease or anemia.
Medications may include topical minoxidil for pattern thinning, prescription options for hormone‑sensitive hair loss, and anti‑inflammatory treatments for autoimmune forms. Ask a clinician about safety if you’re pregnant, trying to conceive, or breastfeeding.
Procedures can include low‑level laser therapy devices that are FDA‑cleared for pattern hair loss, platelet‑rich plasma (PRP) injections, and microneedling in selected cases. For stable pattern hair loss, hair transplantation can be an option after medical evaluation.
When To Seek Medical Advice
Book a dermatology appointment if hair loss is sudden, patchy, rapidly worsening, or paired with scalp pain, burning, redness, or scaling. Those signs can point to inflammatory or scarring conditions that need early treatment.
If shedding started after a major event (illness, surgery, childbirth, weight loss) and is not improving after a few months, an exam can confirm whether it’s telogen effluvium or another condition.
Frequently Asked Questions
What will a dermatologist look for during an exam?
During the exam, a dermatologist checks the scalp for redness, scaling, sores, and scarring, and assesses the overall pattern of thinning. They also look for broken hairs and changes in hair shaft quality.
Your history matters, so expect questions about recent illness, stress, diet, medications, menstrual changes, pregnancy, and family hair‑loss patterns.
What is the most common type of hair loss?
Female pattern hair loss (androgenetic alopecia) is the most common long‑term type. In the United States, androgenetic alopecia is estimated to affect tens of millions of women.
Can vitamin deficiency cause hair loss?
Yes. Low iron stores, vitamin D deficiency, zinc deficiency, and other nutritional issues can contribute to shedding or make thinning look worse.
Because supplements aren’t risk‑free, it’s safest to test first and treat deficiencies with professional guidance.