What Is Coeliac Disease?
Coeliac disease is a chronic autoimmune condition where eating gluten (found in wheat, barley, and rye) triggers an immune reaction. Over time, this reaction damages the lining of the small intestine, which can reduce the body’s ability to absorb iron, zinc, and several vitamins. When nutrient stores drop, hair can become weaker, thinner, and more prone to shedding.
How Coeliac Disease Can Lead To Hair Loss
Nutrient Malabsorption And Deficiencies
Hair follicles are metabolically active, so they are sensitive to low nutrient levels. In coeliac disease, poor absorption may lead to iron-deficiency anaemia, low zinc, and reduced levels of vitamins such as vitamin D, B12, and folate. These deficiencies can push more hairs into the shedding phase (telogen), leading to diffuse thinning across the scalp.
Autoimmune Activity
People with one autoimmune condition have a higher risk of others. Coeliac disease may coexist with alopecia areata, an autoimmune form of hair loss that typically causes round or patchy bald spots. Thyroid autoimmune disease can also occur alongside coeliac disease and may contribute to ongoing shedding if untreated.
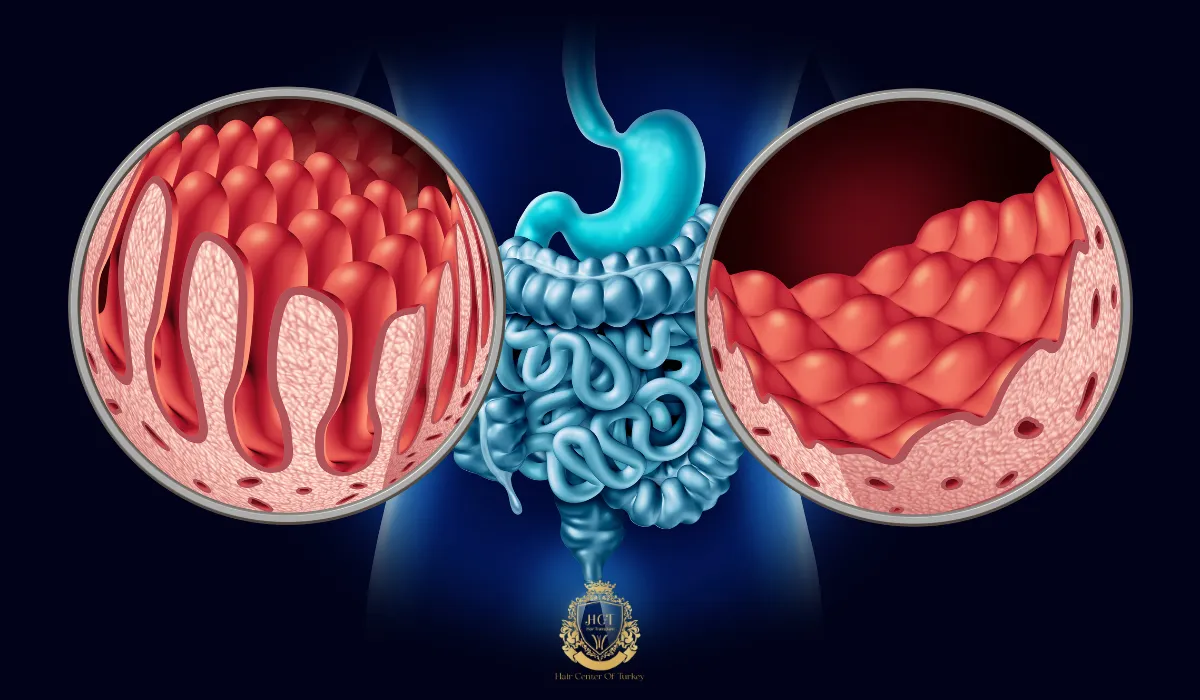
Chronic Inflammation And Scalp Health
Ongoing inflammation can affect the hair-growth cycle and may worsen scalp sensitivity. When the body is under sustained inflammatory stress, it can redirect resources away from non-essential functions like hair production. Some people notice increased breakage or a dull, dry texture when coeliac disease is active and nutritional status is poor.

Signs Of Hair Loss Linked To Coeliac Disease
Common patterns include:
- Diffuse thinning (overall reduction in density across the scalp).
- Excess shedding during washing or brushing.
- Dry, brittle hair that breaks easily.
- Patchy hair loss if alopecia areata is also present.
- Other coeliac clues such as fatigue, bloating, unexplained weight change, mouth ulcers, or iron-deficiency anaemia.
Getting The Right Diagnosis
If you suspect coeliac disease, testing should be done with a healthcare professional. Blood tests often include tissue transglutaminase antibodies (tTG-IgA) alongside a total IgA level; some people may need alternative markers if IgA is low. Diagnosis is commonly confirmed with an upper endoscopy and small-bowel biopsies. Don’t start a gluten-free diet before testing unless your clinician advises it, because removing gluten can make results less reliable.

Managing Hair Loss When You Have Coeliac Disease
Follow A Strict Gluten-Free Diet
A strict gluten-free diet is the foundation of treatment and allows the intestinal lining to heal. Once absorption improves, many people see less shedding and better hair quality over time. Read labels carefully, watch for cross-contamination, and ask for dietitian support if you’re new to gluten-free eating.

Correct Deficiencies With Medical Guidance
Your clinician may check iron studies, vitamin D, B12, folate, and zinc, then recommend supplements if needed. Iron and vitamin D are common targets, but the right plan depends on your labs and symptoms. Avoid self-prescribing high-dose supplements, since too much of certain nutrients can cause side effects or interfere with other minerals.
Reduce Triggers That Increase Shedding
Stress, poor sleep, rapid weight loss, and harsh chemical treatments can worsen shedding. Use gentle scalp care, limit heat styling, and consider a dermatologist review if you have itching, flaking, pain, or visible scalp inflammation. If alopecia areata is present, targeted dermatology treatments may be needed alongside gluten control.
Can Hair Loss Be Reversed?
In many cases, yes. Once coeliac disease is controlled and nutrient levels recover, regrowth often starts within 3 to 6 months, though thicker density can take longer. If shedding continues past this window, another cause may be contributing, such as thyroid disease, androgenetic alopecia, or ongoing iron deficiency.
When To Seek Medical Advice
Arrange a medical review if you notice rapid shedding, bald patches, scalp pain, or hair loss that continues despite a gluten-free diet. Seek help sooner if you have symptoms of anaemia (shortness of breath, dizziness), significant weight loss, or persistent digestive problems. A clinician or dermatologist can confirm the diagnosis and tailor treatment, including checks for thyroid function and other autoimmune conditions.
Frequently Asked Questions
Is hair loss from coeliac disease permanent?
It is often temporary when it’s driven by malabsorption and low nutrient stores. Once gluten is removed strictly and deficiencies are corrected, many people see improvement. Patchy hair loss from alopecia areata may need separate dermatology treatment.
How long does it take for hair to grow back after going gluten-free?
Many people notice less shedding within 3 to 6 months, with continued improvement over 6 to 12 months. Timing varies based on how long coeliac disease was active, baseline nutrient levels, and other health factors.
Should I take biotin for coeliac-related hair loss?
Biotin deficiency is uncommon, but some people still choose low-dose supplements. It’s best to test and correct proven deficiencies first, especially iron and vitamin D. Tell your clinician if you take biotin because it can interfere with certain lab tests.
What else should be checked if shedding doesn’t improve?
A clinician may evaluate thyroid function, iron studies, vitamin levels, hormonal factors, scalp conditions, and family-pattern hair loss. A dermatologist can also assess for alopecia areata or scarring hair loss if patches or scalp changes appear.